For too long, hearing loss has been considered a part of normal aging, and not something that is worth worrying about. Although 30 million Americans have some form of hearing loss, less than 20% wear hearing aids. There is stigma associated with hearing aids which stops many from seeking treatment. This needs to change.

image via
Dementia prevalence is projected to double every 20 years due to the growing aging population of the world. It is incredibly important to identify factors that increase these risks, and identify ways to reduce these numbers. This needs to be a public health priority.
Research by Dr. Frank R Lin, MD PhD and colleagues at Johns Hopkins University has shed light on the independent link between hearing loss and dementia, and the need to treat hearing loss sooner rather than later.
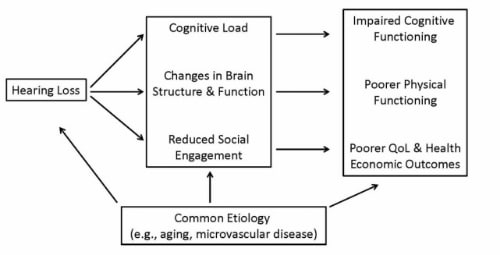
In 2011, the first longitudinal studies came out on dementia and hearing loss, followed in more recent years on cognitive decline and hearing loss (a precursor for dementia), and hearing loss and brain tissue loss. The first study, using data on patients participating in the Baltimore Longitudinal Study of Aging, found a relationship between the risk of all-cause dementia was increased with the severity of hearing loss.
In a second study published in 2011, using a different longitudinal study group, (the National Health and Nutritional Examination Survey) explored a precursor to dementia, cognitive function decline and hearing loss. Lin found that greater hearing loss was significantly associated with lower scores on the Digit Symbol Substitution Test, a nonverbal measure of executive function and psychomotor speed. This study also explored the use of hearing aids in this population. He found that hearing aid use was significantly associated with higher cognitive scores. The reduction in cognitive function associated with a mild 25 dB hearing loss was equivalent to the reduction associated with an age difference of 7 years.
The evidence has continued to mount since these studies were published. I’ve counseled patients for years of the need to re-establish brain pathways once sound is re-introduced through hearing aids. I feel an even greater urgency to diagnose and treat hearing loss as soon as possible.
In 2012, Lin wrote in the Journal of the American Medical Association that compared to patients with normal hearing, those with a mild hearing loss have a two-fold risk of dementia, moderate loss has a 3-fold risk, and that severe hearing loss has a five-fold risk of developing dementia.
image via
Another 2013 study, using a different longitudinal data set found similar evidence. Hearing loss was again associated with greater rates of decline in cognitive function than those with normal hearing. Individuals with hearing loss in this study had a 24% increased risk of cognitive decline. They found that rates of cognitive decline and the risk of cognitive impairment were linearly associated with the severity of the individual’s hearing loss.
Dr. Lin summarized his research thus far:
“Through these studies, we have shown that hearing loss is independently associated with poorer cognitive functioning on non-verbal tests of memory and executive function, accelerated cognitive decline, the risk of developing dementia, and accelerated rates of brain atrophy. “
Hearing loss and cognitive decline and incident cognitive impairment are independently associated, with the risk growing with the severity of the hearing loss. So what needs to be done?
First, we need to advocate for hearing loss prevention and treatment. This begins with the primary care physicians in our area, and grows from there.
Second, make routine hearing evaluations the standard of care for each individual. Annual exams should be recommended for everyone over the age of 50, even younger if hearing loss is documented sooner.
Third, find hearing healthcare providers who not only evaluate hearing, but provide aural rehabilitation. To quote Dr. Lin’s 2013 comments: “Contrary to popular perceptions, proper hearing rehabilitative treatment is complex, does not simply consist of using a hearing aid, and can vary substantially depending on the treating audiologist.”
Just this year, Dr. Lin released preliminary findings with MRI studies that showed there is accelerated brain atrophy in those with hearing loss compared to those without. To quote Lin, “If you want to address hearing loss well, you want to do it sooner than later. If hearing loss is potentially contributing to the differences we’re seeing on MRI, you want to treat it before these brain structural changes take place.”
Hearing loss is a complex issue that takes sensitivity and accuracy to diagnose and treat properly. Diagnostic testing should include not only pure tone testing, but speech-signal based testing and speech in noise testing as well. Treatment with hearing aids is not always sufficient, and aural rehabilitation is an important component that should always be discussed. Hearing aids must also be fit using real-ear or speech mapping to verify fit and quantify benefit. Hearing aids must also be WORN daily to actually get the benefits prescribed by the fitting. Daily checks of hearing aid function should be performed by the patient or care givers to assure proper working order. If hearing aids are worn, but aren’t working, they are essentially expensive ear plugs that can exacerbate cognitive problems and increase social consequences.
Since studying this topic, I am even more excited to see patients and help reverse this trend. Future studies will look at the treatment of hearing loss, and measure it’s worth in preventing cognitive decline. I know that when a complete treatment plan for hearing loss is implemented, including proper aural rehabilitation, lives can be changed. I’m just grateful to be able to be part of the solution.
Sources:
www.ncbi.nlm.nih.gov/pubmed/?term=PMID%3A+23337978
http://www.ncbi.nlm.nih.gov/pubmed/?term=PMID%3A+21320988
http://www.ncbi.nlm.nih.gov/pubmed/?term=PMID%3A+21728425